
- Nipah virus was first identified in Malaysia in 1998-99 among pig farmers and abattoir workers
- The virus likely originated in fruit bats and spread to pigs before infecting humans
- The initial outbreak caused 283 human cases and 109 deaths, with a fatality rate of 39%
With 2 confirmed cases in West Bengal and airports across Asia taking precautionary screening measures, Nipah virus is once again in the news as a major health concern that has the potential to affect millions. But do you know exactly when and how Nipah virus go its recognition as one of the deadliest viral infections to plague the world today? The emergence of the Nipah virus in the late 1990s stands as one of the most important zoonotic disease discoveries of recent decades, shedding light on how viruses can move from wildlife to livestock and then to humans. First identified in Malaysia in 1998-99, the Nipah virus outbreak began among pig farmers and abattoir workers, and triggered a major public health crisis involving hundreds of human cases and the destruction of millions of pigs to halt further spread.
Named after Sungai Nipah, a village on the Malaysian Peninsula where it was first isolated, Nipah virus belongs to the Paramyxoviridae family, genus Henipavirus, the same group that includes the Hendra virus. Initial infections were mistaken for Japanese encephalitis, but scientists soon discovered a novel pathogen causing severe encephalitis and respiratory illness in humans and animals.
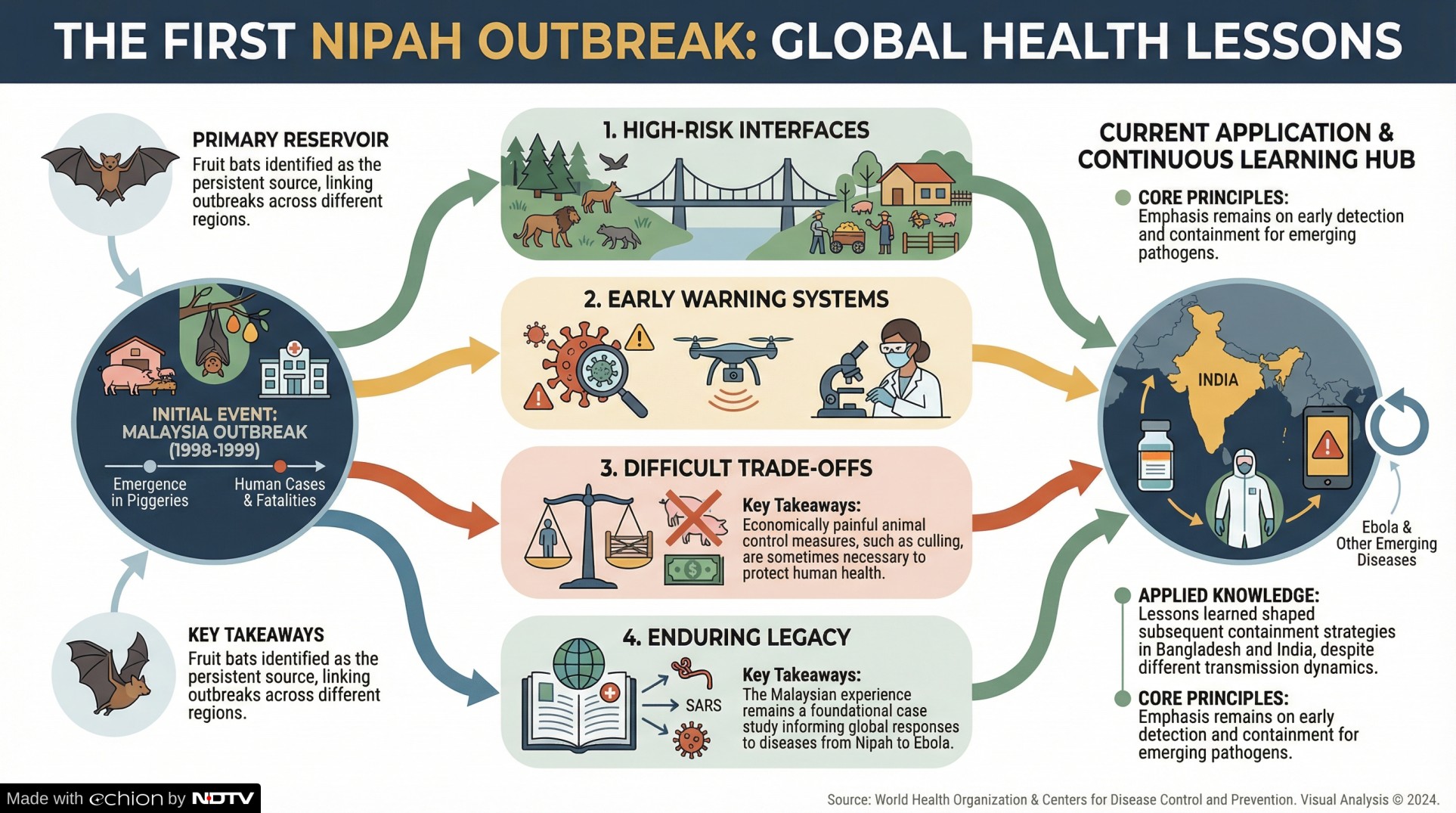
This early outbreak fundamentally changed how scientists and public health agencies view zoonotic threats. It highlighted the dangers posed by close interactions between wildlife and livestock and emphasised the importance of surveillance at the animal-human interface. As emerging outbreaks continue in locations such as West Bengal, Kerala in India and countries like Bangladesh, the lessons from Malaysia remain foundational to global disease preparedness.
The Malaysian Outbreak: How It Began From Bats to Pigs
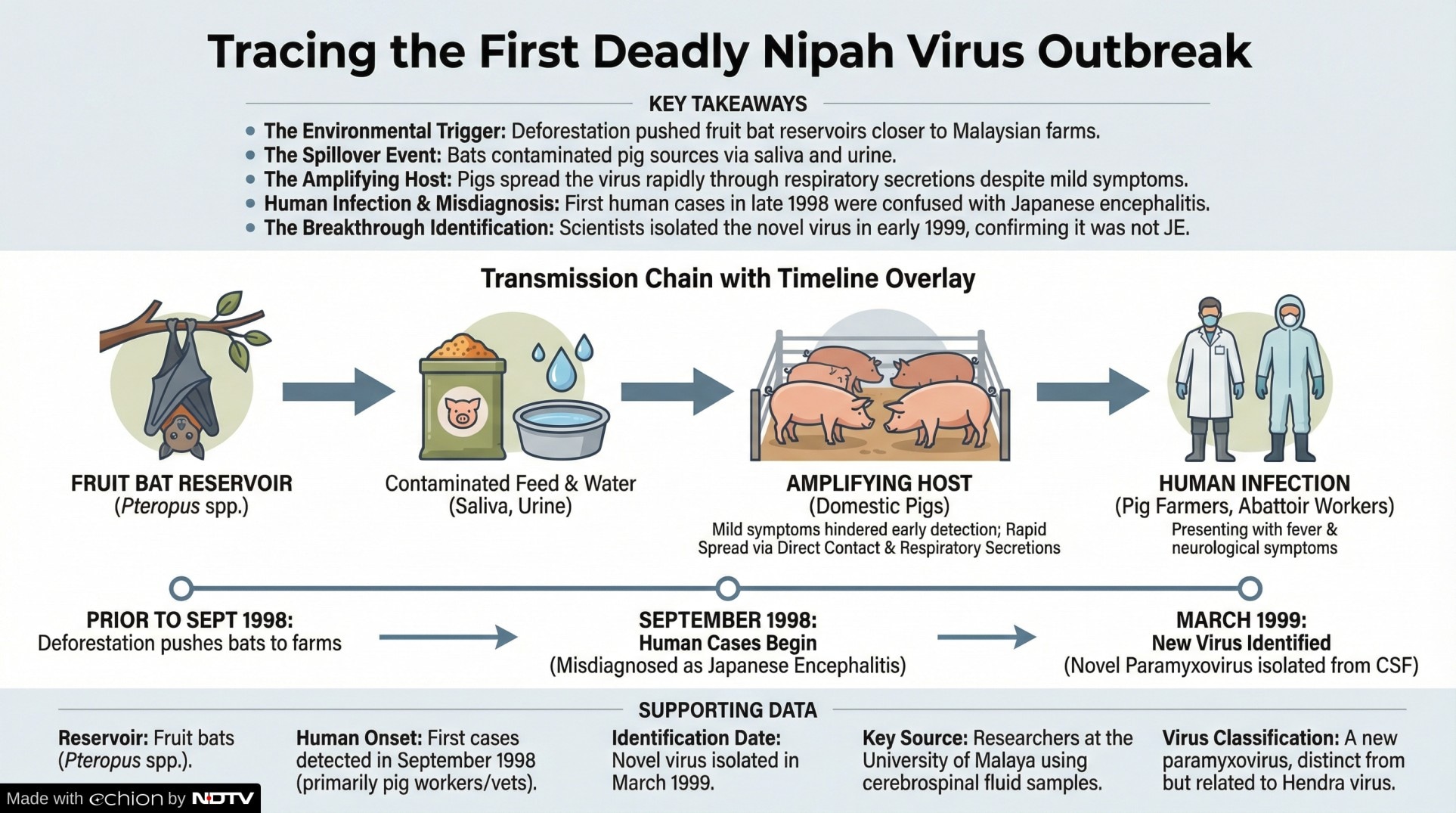
The Nipah virus likely originated in fruit bats (Pteropus spp.), known reservoirs for the virus. These bats can shed the virus in saliva, urine and other bodily fluids. In Malaysia, environmental changes and deforestation pushed fruit bats closer to human settlements and agricultural areas. When bats foraged near pig farms, virus particles contaminated pig food or water, enabling spillover into domestic pigs.
Once in pig populations, Nipah virus spread rapidly through direct contact, respiratory secretions and contaminated materials. Pigs often showed mild or nonspecific respiratory symptoms, which made early detection difficult.
Human Nipah Virus Infections and the First Detection
The first human infections were detected among pig farm workers and veterinarians. Initial cases in September 1998, characterised by fever, headache and neurological symptoms, were initially thought to be Japanese encephalitis, a known viral disease in the region. However, despite control efforts, the outbreak intensified, prompting deeper investigation.
By March 1999, researchers from the University of Malaya successfully isolated a previously unknown virus from patients' cerebrospinal fluid samples. Genetic and structural analyses identified it as a paramyxovirus closely related to Hendra, but distinct enough to designate it as a new virus, Nipah virus, named after the village where it was first identified.
Also Read: Nipah Virus In India: What Is Actually Going On? Timeline Explained
Impact: Human and Animal Toll of the First Nipah Virus Outbreak
1. Human Cases and Fatalities
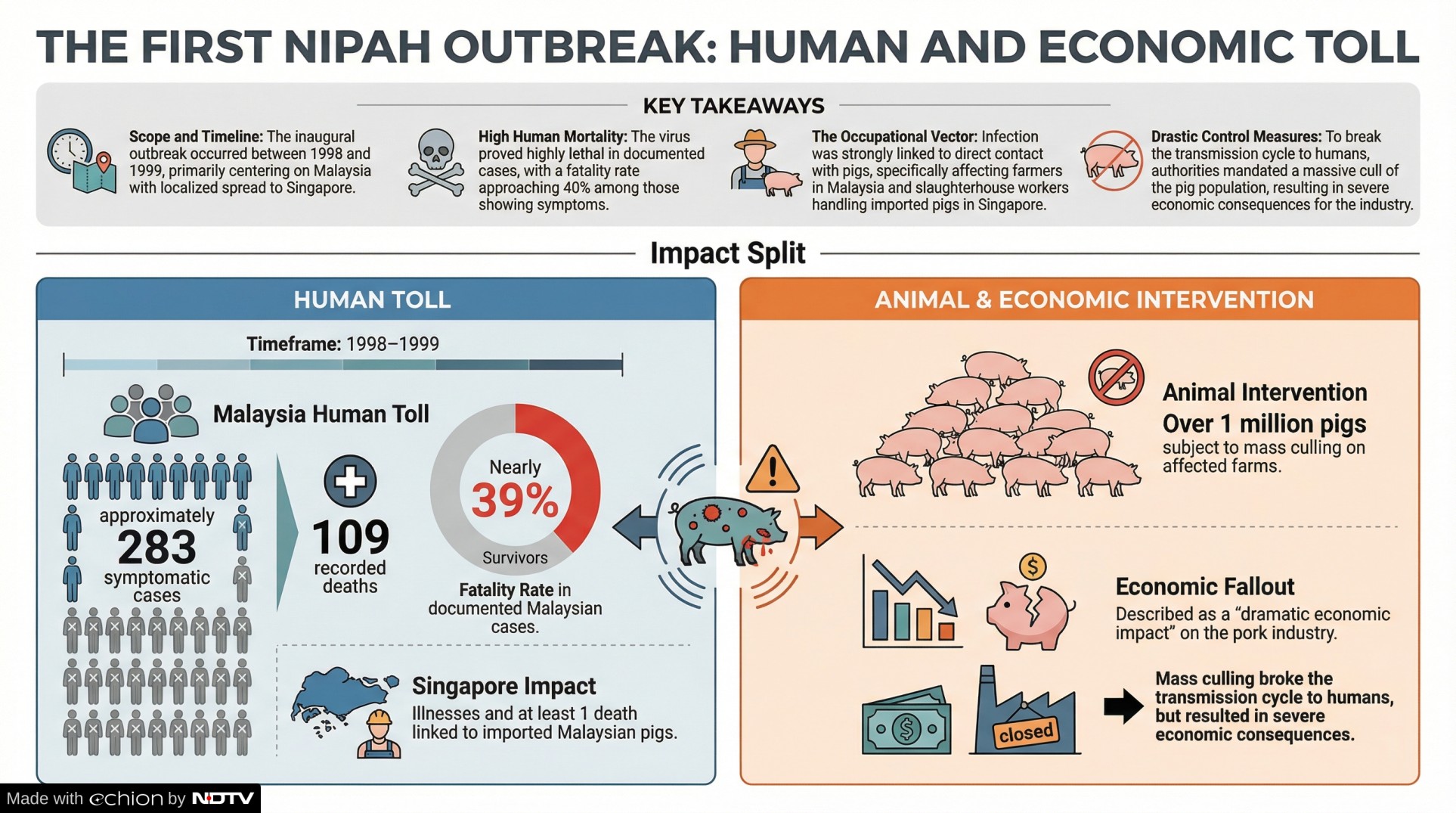
From 1998 to 1999, clinical surveillance recorded around 283 symptomatic human cases of Nipah virus infection in Malaysia, with 109 deaths, a fatality rate of nearly 39% in documented cases. Many of those affected were involved with pig farming or processed pigs as part of their work. A related outbreak also occurred in Singapore within slaughterhouse workers exposed to pigs imported from Malaysia, causing additional illness and at least one death.
2. Pig Culling and Economic Losses
To control the outbreak, Malaysian authorities implemented a mass culling of more than 1 million pigs on affected farms. This was aimed at breaking the transmission cycle and stopping further spread to humans. The culling had a dramatic economic impact on the pork industry but was considered necessary to protect public health.
Recognition For Nipah Virus: Scientific Discoveries and Early Understanding
The identification of Nipah virus triggered extensive scientific research. Analyses confirmed the virus as a member of a new Henipavirus genus, distinct from other paramyxoviruses. Subsequent studies demonstrated that pigs could carry multiple strains of Nipah virus, and that controlling animal movement was key to limiting spread.
Field studies also confirmed that fruit bats were the natural reservoir hosts, with widespread evidence of the virus across bat populations in the region. This understanding helped explain why human outbreaks could occur repeatedly when environmental conditions brought bats into closer contact with domestic animals and humans.
Global Lessons and Long-Term Significance
The Malaysian outbreak reshaped global perspectives on zoonotic diseases. It underscored several key public health principles:
- Animal-human interfaces are high-risk zones for spillover infections.
- Wildlife surveillance is critical for early detection of emerging pathogens.
- Rapid diagnostic investigation is essential when unusual illness clusters arise.
- Culling and other animal control measures, though economically painful, can protect human health.
These lessons have informed responses to later Nipah outbreaks in Bangladesh and India, where transmission dynamics differ but still involve fruit bats as a reservoir and emphasise early detection and containment. As the world continues to confront zoonotic diseases, from Nipah to Ebola and beyond, the Malaysian experience remains a foundational case study for disease surveillance and outbreak response.
Disclaimer: This content, including advice, provides generic information only. It is in no way a substitute for a qualified medical opinion. Always consult a specialist or your own doctor for more information. NDTV does not claim responsibility for this information.
Track Latest News Live on NDTV.com and get news updates from India and around the world

